Now, more than ever, mental health forms a major component of my work in nutrition. The COVID-19 pandemic has led to an unprecedented increase in stress among communities and individuals, worsening or triggering mental health conditions such as depression.
The PHQ-9 screen forms part of all initial nutrition consultations. The PHQ-9 is a simple, 9-question instrument for screening, diagnosing, monitoring and measuring the severity of depression.
PHQ-9 is one of the most used depression screens among Primary Care workers, clinicians and researchers. The assessment is endorsed by a number of leading health organizations, including the National Institute for Health and Care Excellence (NICE). The assessment takes 3 minutes to complete.
The PHQ-9 evaluation, together with the Creyos Health cognitive assessment, gives you a far deeper insight of what is going on with both your cognitive and mental health. These scientifically-validated assessments help further inform your personal nutrition and care programme, providing quantifiable evidence.
How do we evaluate the PHQ-9 Assessment?
We evaluate your PHQ-9 alongside other clinical considerations including the findings from your initial in-depth nutrition consultation. For instance, were your current symptoms triggered by a psychosocial stressor(s)? What is the duration of the present episode and are you receiving any other treatment or support? To what degree are your symptoms impairing your usual work and activities? Is there a history of similar episodes? Is there a family history?
How does depression relate to digestive health and nutrition?
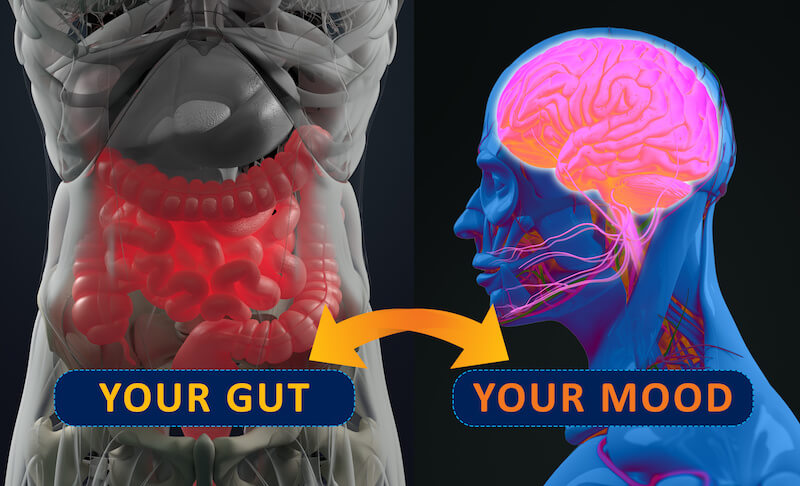
There is mounting evidence that the good bacteria in the gut (our microbiota) influence our brain and our mood. And indeed, it is the food that we eat that determines the types of bacteria that inhabit our gut. Some bacteria are beneficial but others are not and may contribute to inflammation in the body. This is where a targeted and individualised holistic nutrition programme may be beneficial: to help rebalance and strengthen your gut microbiome and help reduce inflammation.
Our gut bacteria produce hundreds of neurochemicals that the brain uses to regulate basic physiological processes as well as mental processes such as learning, memory and mood.. Our gut bacteria manufacture about 95 percent of our serotonin, which influences our mood and sleep patterns.
People with chronic inflammatory diseases such as diabetes, cardiovascular disease and autoimmune disorders are at greater risk of developing depression. Depression can also be one of the symptoms of many inflammatory neurological conditions, such as multiple sclerosis and Parkinson’s disease. Depression may even be a risk in developing Alzheimer’s disease later in life.
How does inflammation contribute to depression?
Studies support that the brains of patients with depression have higher levels of inflammation. Their microglia – the brain’s immune system cells – are also more active. This increased activity could end up being detrimental, leading to changes in how the brains cells function and communicate.
Another study found that people with depression had more neutrophils, lymphocytes, and monocytes and inflammatory proteins in their blood compared to those without depression. This is another indicator of inflammation in the body in general.

Additional benefits of a Cognitive Health and PHQ-9 Assessment
Research shows that even if your focus is not mental health, a quick measure of depression can be beneficial. Depression and cognition are associated with a wide variety of mental and physical illnesses. A study published in JAMA Psychiatry (Sullivan et al., 2013) found that depression was associated with accelerated cognitive decline among type 2 diabetes patients. The greatest decline occurred in patients with a PHQ-9 score of 10 or more at baseline and 20 months later. The researchers propose that depression may be causing or worsening the risk of dementia.
Another study (Hawkins et al., 2016) involved patients with heart failure, who have high rates of depression and cognitive impairment. The researchers found that certain PHQ-9 scores predicted performance in multiple cognitive domains. They suggest treatments known to affect depression and cognition, including CBT and physical exercise, may be most impactful on this population.